An artificial intelligence that can scan sperm to work out which are healthiest has been developed by scientists.
Even in men who eat well and exercise regularly, barely one in ten sperm are healthy — and in some men the ratio falls below four percent.
At the Oma Clinic in California, however, scientists have developed a ‘sperm health test’ algorithm that scans swimmers for their shape and how they move to pick out the best ones for fertilizing an egg from the crowd.
They hope that it will boost success rates with invitro fertilization (IVF) and lower costs, meaning couples will need fewer rounds of the treatment.


To develop the algorithm, the scientists began by extracting a subset of sperm from each sample — which contained up to 20,000 swimmers. They then then placed the samples under a microscope and analyzed the health of each


A healthy sperm has a smooth and oval shaped head, and will also be able to swim rapidly and in a straight line but doctors behind the AI said that finding these swimmers is often like searching for a ‘needle in a haystack’
Dr Kiran Joshi, an entrepreneur who helped develop the AI, told DailyMail.com: ‘As it stands right now, couples have to go through three cycles of IVF on average.
‘We want to reduce that number as that will reduce the pain and reduce the financial burden and lead to more success.’
About 40 percent of infertility cases are down to the male partner, studies suggest, with sperm counts having been in freefall for decades — a pattern blamed on the rise of poor diets and sedentary lifestyles.
Dr Joshi explained to this website that the algorithm had been built by scanning sperm from the ejaculates of more than 1,000 men.
The samples were submitted by fertility clinics across the US and other countries, and were mostly from men in their 30s and 40s — although they ranged up to the age of 75 years.
To develop the algorithm, the scientists began by extracting a subset of sperm from each sample — which contained up to 20,000 swimmers.
Top embryologists then placed the samples under a microscope and analyzed the health of each.
They were graded based on two factors: Their shape and how well they swim.
A healthy sperm has a smooth and oval shaped head, and will also be able to swim rapidly and in a straight line.
But Dr Joshi said that finding these swimmers is often like searching for a ‘needle in a haystack’.
Explaining what it is like analyzing a sample, Dr Michael Guarnaccia, an embryologist who was also involved in developing the AI, said: ‘We have some sperm who swim in non-straight patterns, and sometimes we see sperm swimming in circles or in an aberrant way.’
The sperm were graded based on these two aspects using standardized measures and an about ten second video of each was then recorded.
This was then fed into the AI to give it the ability to accurately estimate how healthy any one particular sperm is.
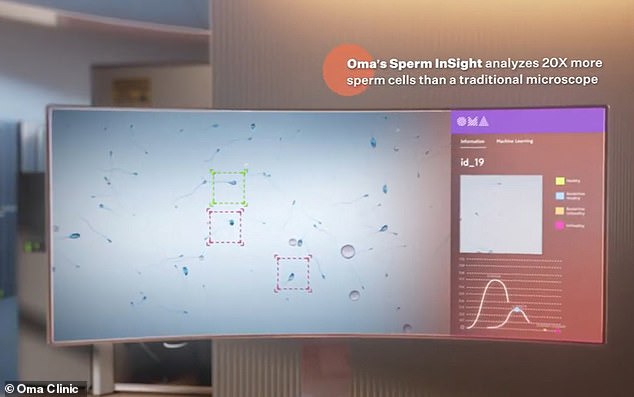
When the AI is in use, it draws a box around each sperm and then quickly allocates a color based on the perceived health of the sperm.
Results are delivered within seconds — with red boxes indicating unhealthy sperm and green indicating those which are healthy.
The scientists are set to publish their research in an academic journal over the next couple of months, although they are unable to say in which one.
They have carried out tests monitoring the success rates of IVF rounds that have used and have not used the technology.
At this stage, the researchers cannot reveal the results, but said that there was a ‘significant’ difference between the two groups.
Dr Guarnaccia told DailyMail.com: ‘We did show an increase in the percentage of fertilization and the rate of advancing embryo development.
‘There was a percentage increase both in the fertilization rate and the number of embryos that made it through. That was statistically significant.’
The technology could mark a significant step forward for the IVF industry, by boosting fertilization rates and reducing the costs and time needed for couples to go through the process and conceive.
It may also help scientists by giving them a second opinion, with some experts contending that it is often a struggle to tell apart the healthy sperm.
About 36,000 children are born via IVF in the United States every year, estimates suggest, accounting for one percent of all births.
But this is a figure that continues to rise as more couples leave starting a family until later in life. Estimates suggest that by 2050 as many as half of all babies may be born in the US via IVF treatments.
This post first appeared on Dailymail.co.uk