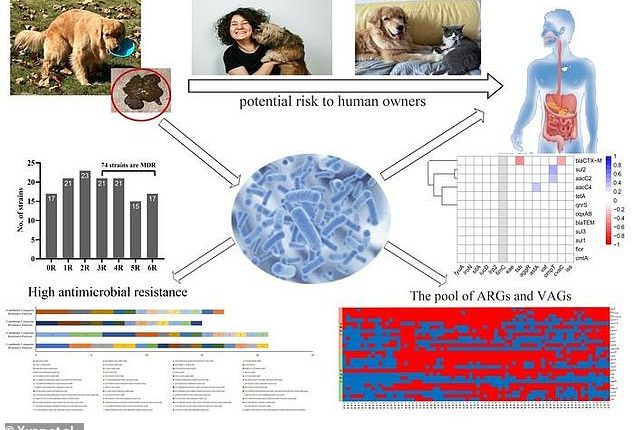
More than half of pet dogs are harboring an antibiotic-resistant superbug that is easily transmitted to humans, a new study has revealed.
A team of Chinese scientists found most dogs suffering from diarrhea are carrying multi-drug resistant strains of Escherichia coli (E. coli), an intestinal bug that does not respond to some or all antibiotics.
Humans infected with E.coli can experience diarrhea, stomach cramps, fever and, in rare cases, kidney failure and death.
The team tested feces samples from 135 pet dogs who were having diarrhea, finding that more than 50 percent of the canines were carrying the bacteria.
Drug-resistant superbugs are likely becoming more common because of the widespread use of antibiotic drugs in agriculture and medicine, the scientists behind the new work concluded.
Pet dogs with diarrhea may be shedding multi-drug resistant E.coli in 5 in 10 cases, with potential risks to their human owners.


Your companion animal could be carrying antibiotic-resistant superbugs – bacteria that can’t be treated by conventional antibiotics.
This overwhelming presence of superbugs among companion animals could accelerate the emergence of new drug-resistant diseases in people, the scientists wrote.
Superbugs kill over one million people each year, according to the World Health Organization (WHO). The organization has warned that the planet is heading for a ‘post-antibiotic’ era.
As many as half of multidrug-resistant infections are actually acquired in the hospital, one large-scale study found.
A post-antibiotic era would effectively turn back time, putting us in an era when a simple surgery or a scrape could become a life-threatening medical emergency.
And according to the new study, dogs may play a role in spreading these dangerous bacteria.
Scientists took 185 feces samples from dogs who had confirmed cases of diarrhea over a one-year period.
Dogs that had taken antimicrobial drugs of any kind in the past three months were excluded to make sure they were getting a relatively un-altered look at their bacterial contents.
The team then extracted and cultured the E. coli bacteria from the samples, ending up with 135 that they grew in dishes for further testing.
They then tested 16 different antibiotic drugs, comprising six categories of drug, on each sample to see which ones were effective.
Between 59 and 76 percent of the samples contained bacteria that were resistant to an entire class of drugs.
Specifically, 59 percent of the samples were resistant to sulfonamides, 64 percent were resistant to tetracyclines, and 76 percent were resistant to beta-lactams.
These three classes include the most commonly used antibiotic drugs.
‘The widespread use of antibiotics has significantly caused the increase of[multi-drug resistant] E. coli which were isolated from companion animals,’ wrote the team, from the College of Veterinary Medicine at Sichuan Agricultural University.
Antimicrobial chemicals in everyday items like hand soap, too, have been linked to rising rates of drug resistant bacteria, as has the use of alcohol and bleach for disinfecting homes and hospitals.
Part of what makes E. coli resistant to antibiotics is an accelerated form of evolution – survival of the fittest.


E. coli is a type of bacteria that exists natural in our intestines, as well as in dogs’. But too much of it can make us sick, and E. coli is increasingly resistant to common treatments.


Disinfectants and antiseptics are commonly used to clean surfaces, surgical instruments and even skin across healthcare settings. But these could increase antibiotic resistance when they leave survivors behind.
When a dog or human is treated with an antibiotic, harmful bacteria are killed off.
But it may not be 100 percent of them.
The ones that survive are able to survive because they have specific genetic variants that give them protection against antibiotics.
When these bacteria survive, they pass on their resistance genes to their offspring.
Not only that, but bacteria can also share genetic material with each other. That means they can give each other resistance genes without even reproducing.
In recent years, restrictions to antibiotic prescribing have sought to improve the situation, but according to the new study, the problem may be too far gone to control.
The high detection rates of [multi-drug resistant] E. coli in our study implied that more effective measures should be taken to control the occurrence and spread of [multi-drug resistant] E. coli from companion animals,’ the researchers wrote.