WASHINGTON — Last year on Christmas Eve, advisers to then-President-elect Joe Biden held an emergency meeting to discuss a scenario that felt increasingly likely: the emergence of a mutant strain of the coronavirus that would evade vaccine protection.
At the time, the alarm bells were ringing for the alpha variant, which quickly faded. But the concerns led Biden’s team to lay the groundwork for the plan they are now beginning to implement as researchers work to determine how much of a threat the omicron variant may pose, according to people familiar with the planning.
While there are still more questions than answers about the variant, Biden administration officials are prepping for a litany of worst-case scenarios and daunting questions, such as: What would happen if it turned out more than 200 million Americans needed to be revaccinated?
It will be several weeks before officials know the answer to that question. So far, they have said it is possible booster doses of the current vaccines will provide enough protection if the omicron variant turns out to be more lethal or contagious.
But until they know for sure, they are also counting on a system of genomic sequencing and testing the administration has spent billions of dollars building out since President Biden’s early days in office to help keep schools open and prevent the economy from another shutdown.
“We are equipped and prepared to fight the omicron variant head on,” CDC director Rochelle Walensky told reporters Friday. “We are actively taking steps to stay ahead of the omicron variant.”
A central piece of the plan will be to quickly modify and manufacture new vaccines tailored to address a specific variant should the need arise. Since the early days of vaccination efforts, administration officials have been working with vaccine makers to ensure those companies could rapidly reformulate the existing vaccines, get them through the regulatory process and begin mass production in a matter of months if needed.
Those conversations went into high gear the week of Thanksgiving when the first infections of the omicron variant were confirmed in South Africa, White House Covid coordinator Jeffrey Zients said.
“These conversations are happening as we speak in the spirit of being prepared for any scenario,” he said.
To ensure the U.S. would still have enough vaccine supply, the administration included an option in a July contract with Pfizer that would enable purchase of an updated version of the vaccine for a potential variant or a new formulation.
Pfizer and Moderna, which began working on an omicron vaccine last month, have already been through the process of reformulating their vaccines for the beta and delta variant even though new vaccines were never needed for those strains.
They were able to make new vaccines for each variant, but never brought the vaccines to market because the beta variant died off and with delta, the booster shots of the current vaccine appeared to be just as effective as a new delta-specific vaccine.
If needed, the time to get a new vaccine to market could be less than 100 days and new shots could be going into arms in the first quarter of 2022, said Andy Slavitt, who served as a top White House advisor on the pandemic through June.
“The good news is, in the event new formulations were needed, with the mRNA vaccines, you can change the production to a new vaccine on a dime,” Slavitt said.
But he noted that boosters are likely to also provide protection against the new variant, meaning the biggest task ahead might be convincing the 100 million Americans yet to get their booster to line up for a third shot in the weeks ahead.
Even if it is determined that previously vaccinated Americans need to be revaccinated, health officials said they aren’t anticipating a return of spring’s mass vaccination centers and long wait times for appointments. There are now 80,000 retail pharmacies, and health care providers set up to provide vaccinations, and the distribution, storage, and manufacturing kinks of the early days have been worked out.
“We know what works. I mean, we literally have the written plans, staffing strategies, agreements or arrangements in place,” said Jim Blumenstock, senior vice president for pandemic response and recovery at the Association of State and Territorial Health Officials. “The playbook is there. It’s an issue of just having enough stamina and resources heaven forbid if we had to repeat the whole campaign again.”
But despite nearly a year of planning for the worst, the administration’s response hasn’t been without hiccups. The U.S. was slightly behind other countries in putting a ban on travel in place from the southern African countries where the variant was believed to be most widely circulating. The administration waited a week to change a testing window for international travelers from 72 to 24 hours while officials debated internally the need for stricter travel requirements.
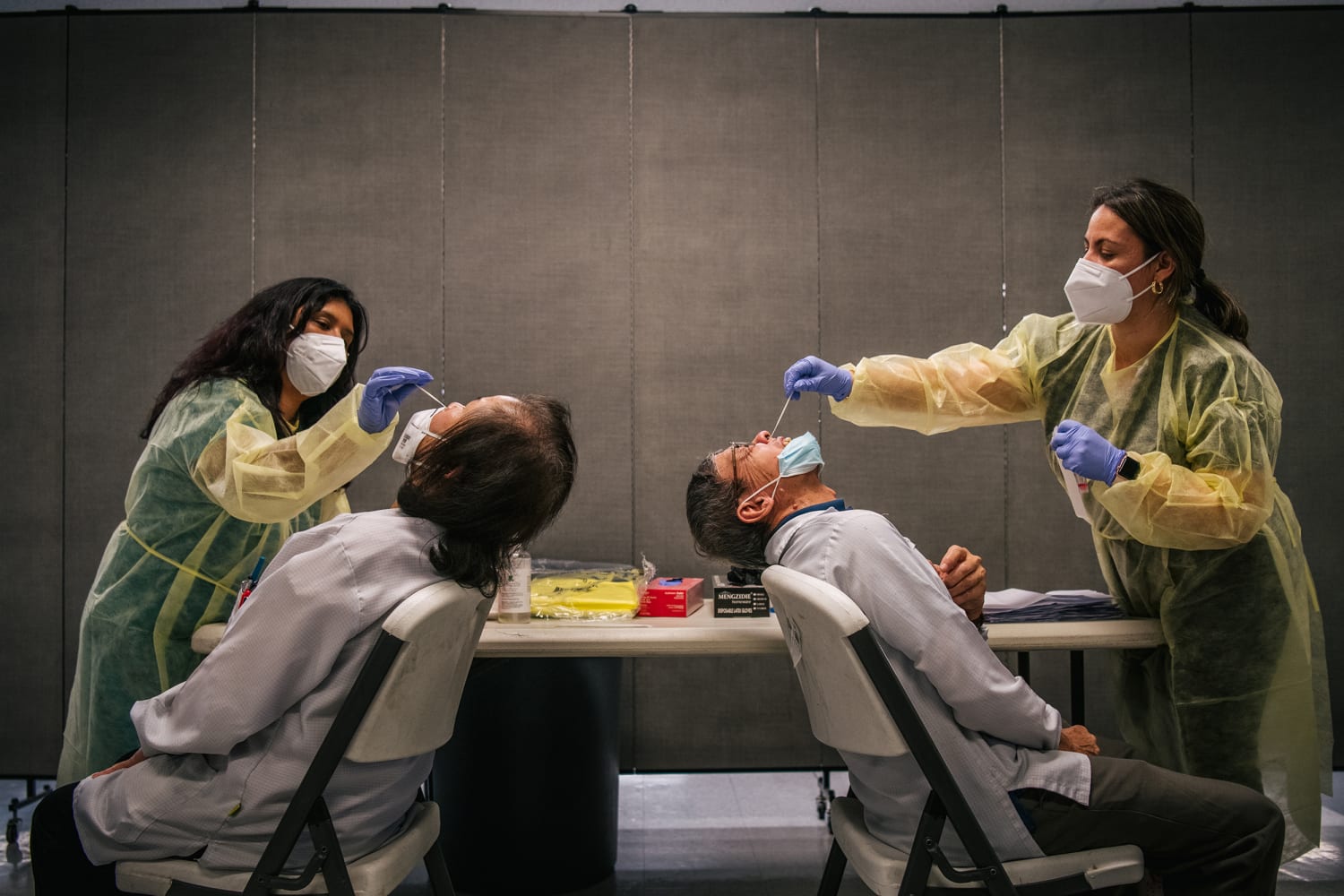
And holes in the ability to respond still remain, starting with the limited supply of rapid tests that can be done at home and provide results in minutes, said Blumenstock. He said state officials repeatedly say they don’t have enough supply to meet the demand for the rapid tests, which is only growing as public health experts urge more Americans to rely on the tests if they are having mild symptoms, around travel or before attending indoor gatherings.
Administration officials have been working for months to try to fill that hole, including spending more than $3 billion in the fall on at-home tests for food banks, health centers and schools — an investment that was also intended to push the test makers to ramp up the scale of production. The U.S. is now on track to have 200 million to 500 million at home tests available each month.
Biden said last week the federal government would require health insurers to reimburse for at-home tests as they would for laboratory tests, though the process for patients to submit claims for the tests and wait to get reimbursed stands to be cumbersome. For those without insurance, the administration will donate 50 million tests to community health clinics.
The administration is also relying on the network of genomic sequencing it has built up to be able to detect concerning variants and hopefully isolate those infected with them and their close contacts. The U.S. has gone from sequencing about 8,000 samples per week at the start of the year to 80,000 samples per week, about 1 in every 7 positive PCR test results.
The first case in the U.S. was identified through genomic sequencing at the University of California in a laboratory that is funded by the CDC using dollars from the Covid relief plan Biden pushed to get passed in the spring.
“The rapid turnaround and sequence analysis is an example of the importance of our investments this year to expand genomic sequencing across the country,” Walensky said Friday. “And to build a system that is prepared to swiftly respond to new and emerging Covid variants.”
Source: | This article originally belongs to Nbcnews.com