The Vanderbilt University Medical Center in Nashville is feeling the effects of an overwhelmed system.
The hospital typically receives referrals from about a 200-mile radius. But increasingly, that treatment area has more than doubled, to a 500-mile radius.
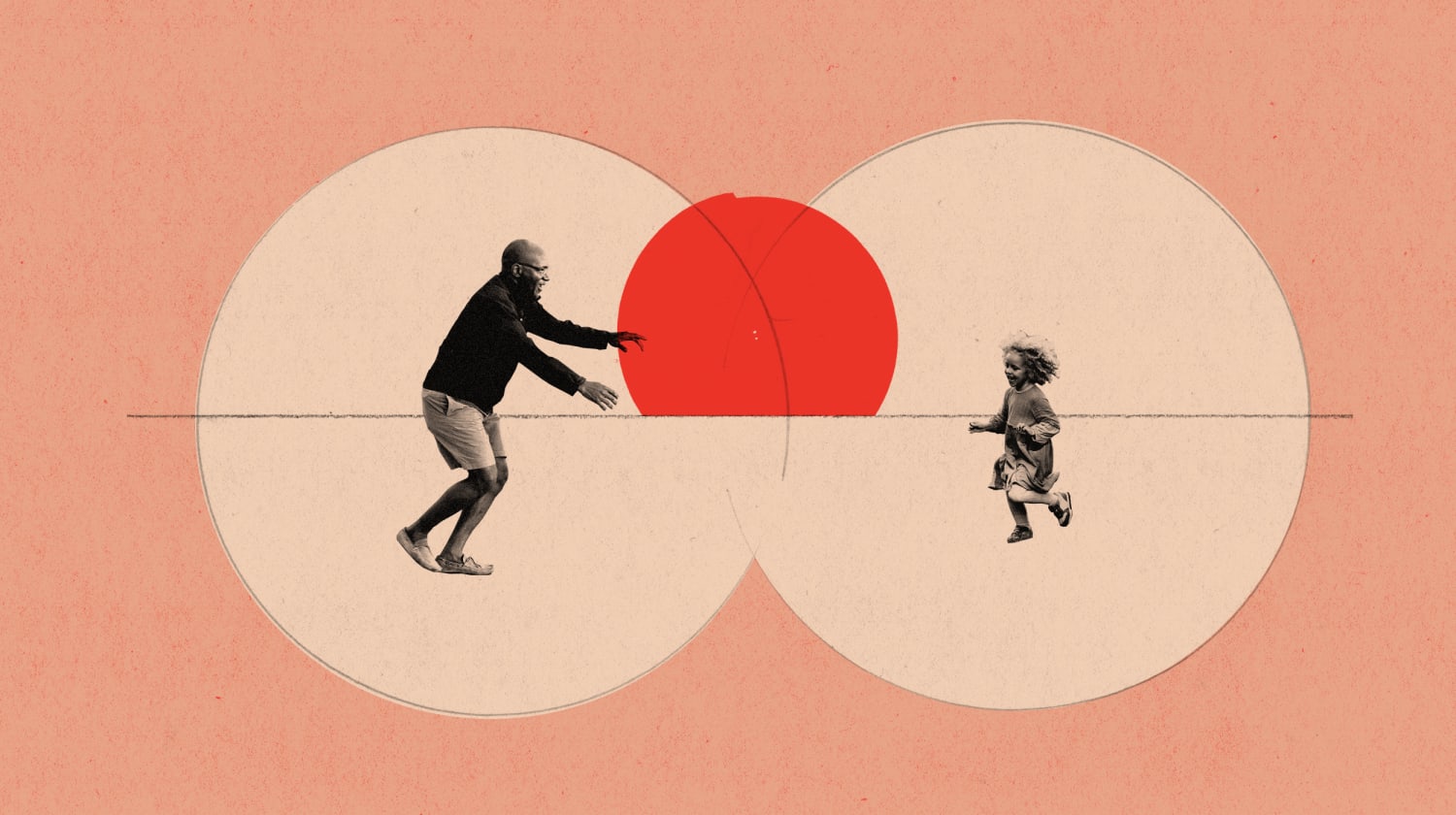
“The circle has just gotten bigger because there aren’t any other available options,” Dr. Todd Rice, the director of Vanderbilt’s medical intensive care unit, said. Rice said one patient traveled eight hours to his facility for care because no closer hospital had the appropriate resources.
The increase in patient load worries critical care physicians like Rice, who say exhausted health care workers will not be able to continue high levels of care into the new year. The number of Covid-19 patients in the Vanderbilt system is projected to swell by another 40 percent in the coming weeks and months.
Dr. Jeff Pothof, chief quality officer and emergency medicine physician at UW Health in Madison, Wisconsin, said his hospital system is so overwhelmed, that his team has had to redirect some Covid-19 patients to makeshift “field hospitals” in the local exposition center, normally used for the Wisconsin State Fair. These are patients who are on the road to recovery, but still require oxygen support before they’re able to be sent home.
Other than during times of natural disasters, such as hurricanes or tornadoes, Pothof said field hospitals in the U.S. are “new territory.”
The United States spends more money on “health care than any other country,” he said. “You just shake your head and wonder: how did we get to the point where, here in the United States, we need to turn exposition centers into field hospitals?”
“We are putting Band-Aids on the system now,” Rice said, warning that “we’ll pay for it in the safety of patients.”
“Medicine is a lot of attention to detail. When you get overwhelmed with work, you tend to be less able to pay attention to detail,” he said.
‘Help lessen the load’
A common approach to treating viruses is to give treatments as early as possible, when there’s a lesser amount of virus in the body, making it easier for drugs to vanquish it. It’s why, for example, the antiviral drug Tamiflu is meant to be given within 48 hours of a person coming down with the flu.
But drugs like this — which could prevent people from being hospitalized in the first place — are in very limited supply for Covid-19.
Though progress has been made on therapeutics — with one authorized drug, the steroid dexamethasone, shown to help severely ill hospitalized patients, and another, Gilead’s remdesivir, which has been approved by the FDA, which may shorten hospital stay — the FDA has authorized just two therapies designed to keep Covid-19 patients out of the hospital.
The treatments — monoclonal antibodies from drugmakers Regeneron and Eli Lilly — are meant to mimic the body’s immune response to SARS-CoV-2, the virus that causes Covid-19, and are authorized for patients at high risk of getting much worse and needing hospitalization.
Regeneron executives have said the company has 80,000 doses ready now for distribution, and will ramp up to 300,000 doses in January. Eli Lilly anticipates it will supply the U.S. with 350,000 doses of its monoclonal antibody treatment by the end of this year.
But the supply so far of either treatment is not enough to meet demand.Over the past week, the average number of daily cases has surpassed 200,000. And the treatments must be given early, before a patient is sick enough to require hospitalization. That means testing must be readily available, with results delivered quickly.
The monoclonal antibodies are a “really big deal” to Shawna Differding, a Covid-19 outpatient coordinator for Sanford Health in Sioux Falls, South Dakota. “Our hospitals are busy. They’re full of Covid patients.”
“I think this option will help lessen the load on the hospitals if we can get it to patients.”
If patients can get it is key. Azar said Wednesday that 278,000 courses of the drugs have been allocated across the country so far.
Saag estimates that he only has enough of the infusions to treat about 1 to 2 percent of his patients who could use it.
Download the NBC News app for full coverage of the coronavirus outbreak
“We only have enough supply to treat a couple people a day,” he said, adding that his outpatient clinic in Birmingham sees about 12 people who might benefit from the treatment every day.
Work is still being done, as well, on treatments for hospitalized patients.
Dr. Andre Kalil, an infectious disease expert at the University of Nebraska Medical Center in Omaha, has been a principal investigator for studies combining remdesivir with the other drugs. The goal is to ward off severe complications of Covid-19, or at least help patients recover more quickly.
Kalil said his research, sponsored by the National Institutes of Health, will continue in 2021 — combining remdesivir with drugs that might extend those benefits, including a multiple sclerosis drug called interferon beta-1a.
“We’ll keep going as long as we see people who are still affected and dying from this disease,” he said. “We have to keep going.”
‘What we do right now’
Dr. Jessica Gold, an assistant professor of psychiatry at the Washington University School of Medicine in St. Louis, is finally able to see a light at the end of the tunnel.
“The vaccines give me hope, because it feels like there’s something to look at on the horizon and say ‘this might have an end,'” she said.
“We’ve been in a sea of uncertainty for a while,” she said. “Anxiety thrives on uncertainty.”
The vaccines give me hope, because it feels like there’s something to look at on the horizon and say, ‘This might have an end.’
But how 2021 plays out still “depends, to a large extent, on what we do right now,” Besser said. The advice is a familiar refrain: wash hands regularly, wear face coverings, congregate when necessary outdoors, and keep physical distances of at least six feet from those outside your household.
“We’re going to have to adapt to Covid for at least the next year,” Dr. Yvonne Maldonado, an infectious disease expert at Stanford Medicine, said. This includes treating masks and social distancing like other safety precautions.
“We are so accustomed to stopping at a red light, even when it’s the middle of the night and there’s nobody in the street,” Maldonado said. “Why do we do that? Because we recognize it’s a societal good.”
Source: | This article originally belongs to Nbcnews.com